Questions My Friends Ask | Part 2: Selecting a Test Type
Which test is best? It depends on why you’re testing and what you need.
December 2022: Whenever you test yourself for COVID at home — whether you’re positive or negative — you should report your result. The results are kept private and anonymous. Every test that gets reported helps public health teams better understand where outbreaks are happening, so they can get help to people who need it.
August 2022: This post has been updated to reflect changes to CDC and FDA guidelines.
Last time, I wrote about my smart friends who still have a lot of questions about COVID-19 testing. In that article, I didn’t even get to the most common question I’m asked: “Which test is the best?”
Because of the way tests work, there’s no single test that’s always the best. So the better question might be, “Which test is the best one for my circumstances?" and that depends on your situation and your priorities. Does it make sense to use the most sensitive test? The one with the fastest result? Is cost a factor? Do you have to use a particular type or even brand of test? All these additional questions are a big part of what makes testing confusing for so many people.
With that in mind, I will dedicate today’s article to answering:
What kind of test should I use if…?
. . . I woke up with a scratchy throat (or some other COVID-19 symptom)? I think it’s allergies or a cold, but could it be COVID-19?
My friend, Sara, texted me this the other day. She wanted to know if she should still attend a birthday dinner with 10 of our friends that evening, and if so, should she get a test first.
This is what at-home tests (rapid antigen tests) were made for: quickly diagnosing cases in people who are sick.
Her test came back negative, which prompted a secondary question…
Should I take my home test results at face value?
These tests rarely provide false positive results, so if you have symptoms or other reasons to suspect you might have COVID-19 and you test positive, assume that the test is accurate and act accordingly.
Negative results are another story. At-home tests may not pick up infections during the first few days. So in Sara’s case, the best thing to do is to retest 48 hours later to make sure. That’s called serial testing, and it’s why most home tests are sold in sets of two. In the meantime, consider quarantining. If you have to interact with others, mask up for everyone’s safety. Even if you don’t have COVID-19, you might prevent the spread of a cold or other virus!
. . . I just attended a large concert (or other indoor event), and now I feel a little awkward about showing up to other in-person commitments this week.
You’ll never go wrong asking what your host or other attendees would prefer. Depending on the sort of activities you have scheduled, you may decide to mask indoors (your most protective strategy after vaccines and boosters) and/or social distance.
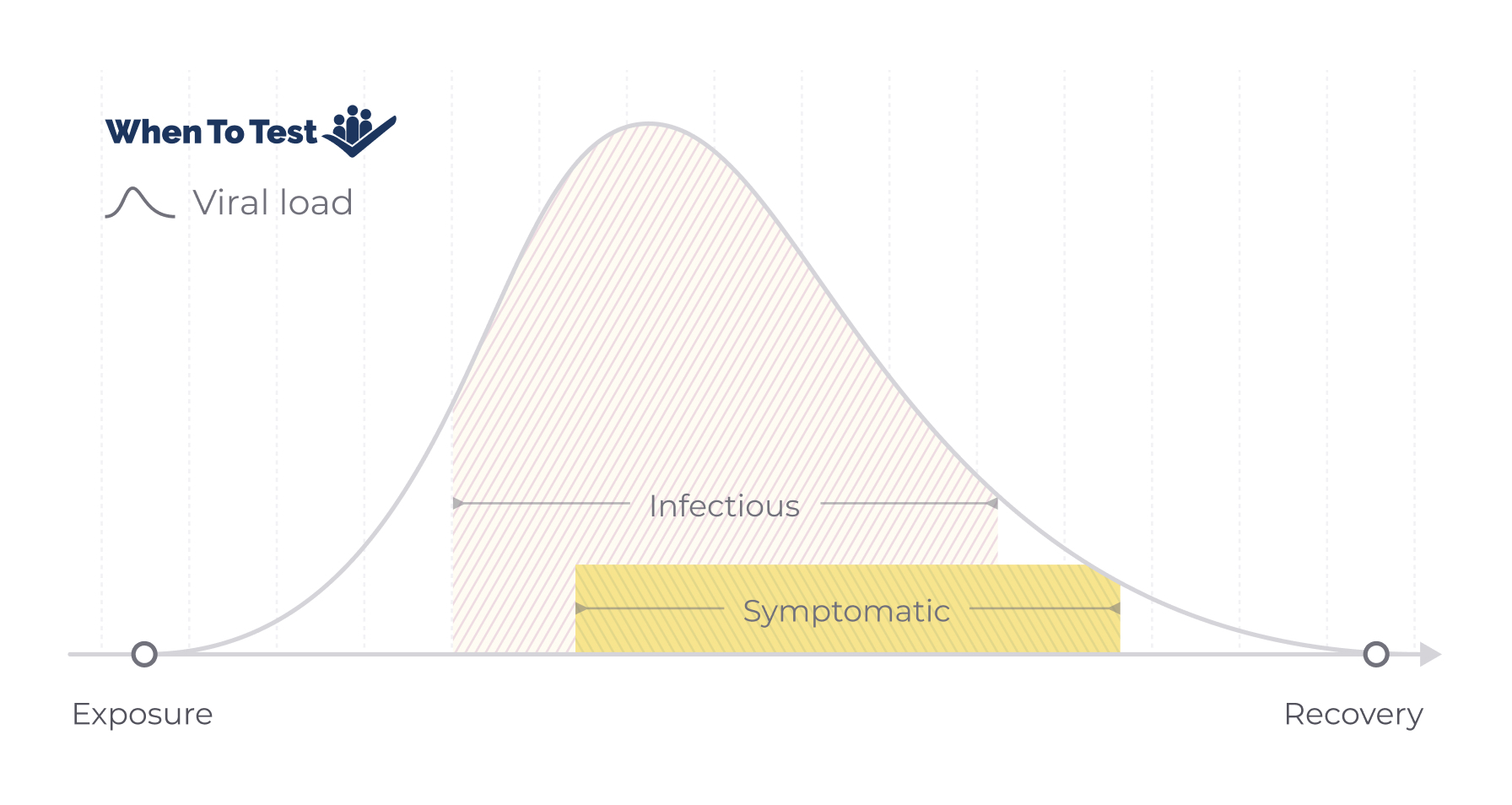
Depending on when this event took place, it may be too early after your exposure for you to be contagious. View this illustration of how COVID-19 behaves to understand the window in which transmission typically occurs.
If the event you went to was less than four days ago, I recommend PCR. An antigen test is unlikely to pick up a positive case until that point. (There’s one exception to this advice: If you’ve also had COVID-19 in the last 90 days. In that case, you should not get a PCR test, because you can continue to test positive even though you’re no longer contagious.)
Once four days have passed, you can go ahead and use an antigen test. But remember, you may not have that much virus in your system yet — in the curve above, you could still be near the beginning of the uphill section. So the first test you take could be negative. To be safer, take at least one more antigen test, 48 hours later. If you can manage it, three tests, with 48 hours between each test, is actually best. If you don’t have symptoms and you test negative all three times, you can be 90% certain that you’re not infected.
. . . I’m going to a major indoor sporting event (or a concert, expo, or other large event)
Check your ticket or the venue’s website for COVID-19 safety requirements. If you are fully vaccinated, testing usually isn’t required. If you’re not vaccinated, many venues will accept negative test results instead. Check which type of test you need (PCR may be required) and the time window for testing (typically within 24-72 hours of the event).
If a test is not required, but you’re considering a test just for good measure, consider your reasons. Do you have symptoms? Do you have reason to believe you might have been exposed recently? Is the prevalence of COVID-19 high in your area? If the answer to all three is “no,” I might suggest just masking instead. A mask — particularly an N95 or KN95 one — will provide you and those around you a measure of protection.
With regard to testing, as we discussed in Sara’s case at the top of this article, a home test (antigen) will not provide an immediate, definitive, negative result. And a PCR test is perhaps a more time and labor intensive process than is justified if you have no reason to believe you may be infected (and may also detect a previous infection rather than a current one).
. . . I’m hosting a ladies’ weekend out of town next month. Should I ask everyone to get tested beforehand?
My friends and I took a trip together in January 2022, when Omicron B.1 was raging through the US. The decision about testing is entirely up to you, but here are some factors you might consider:
How high are the COVID-19 Community Levels in the areas where people are from? If they’re very low, there’s a limited chance of anyone bringing COVID-19 with them. If they’re high, testing becomes more important.
Is everyone fully vaccinated, and are they up to date on their boosters? If they are, the risk that anyone might get seriously ill is lower.
Is anyone in the group at high risk for severe COVID-19?
We had an immunocompromised friend in our bunch, so we all agreed to get tested within a couple of days of attending. This made us feel more comfortable in our carpools and room shares.
If you do decide you want your guests to test, a special touch would be to drop off or mail home tests to the friends who will attend.
. . . I’m visiting my elderly mother (or sick relative, or other high-risk individual) and I want to be as careful as possible?
In this case, being extra-careful means getting a PCR test as close as possible to the time when you will see this person. Because results may take a while to come back, you may want to use a premium service that expedites your results. You can also get tested earlier and then try to limit any chance of exposure between the time you take the test and the time of your visit. But that can be difficult if you will be flying on a plane or using shared transportation to reach them.
Since your interest is being as safe as possible, you will of course consider more than testing. You’ll want to avoid high-risk activities like eating in a restaurant or drinking in a bar the week before you see them, especially if the prevalence of COVID is high in your area. When you’re indoors in public, you’ll want to mask, and practice social distancing to the best of your ability indoors and out. And if transportation will put you in a position to be exposed immediately before seeing them, use masks and practice social distancing with this person until you’ve retested post-exposure.
Should I make my unvaccinated friend get a COVID-19 test in order to come to my wedding?
This question from a soon-to-be bride friend blindsided me! My first instinct was to say that this is completely up to the couple, but then a few supporting questions came to mind.
Are the wedding festivities indoors or outdoors?
What is the COVID-19 Community Level around the time of the wedding? If it’s high, that makes a better case for testing.
Will there be attendees at the wedding who are at risk of getting severely ill from COVID-19?
Are COVID-19 treatments readily available should any high-risk guests require them?
How comfortable do you think other guests will be with having an unvaccinated attendee among them?
Ideally, a good friend will not balk at being asked to take a test to make your special day a little less stressful. And it’s up to you what kind of test you request in this case. For an event of this kind, you might even offer a basket of rapid antigen tests at the entrance for anyone who wants the reassurance.
Have I answered your COVID-19 testing questions yet? Share any other questions you have by emailing me at knoble@whentotest.org, and I’ll try to answer them in a future installment.